BRONX BASEL is a self-guided tour with various activations mapped out within Fordham Heights.


BRONX BASEL is a self-guided tour with various activations mapped out within Fordham Heights.
There is no excerpt because this is a protected post.

For World AIDS Day consideration: Body Hack presents Nuestros Lazos Festival, Dec 1-4

Taking medication is not without risks, especially for the elderly.
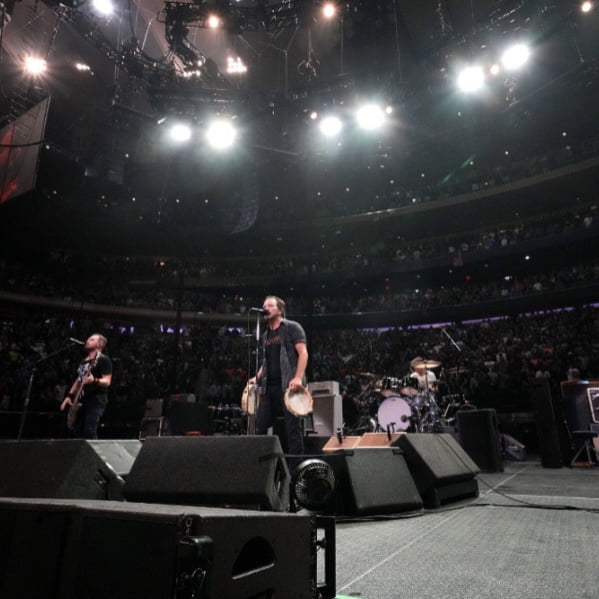
Pearl Jam Calls for September 12th Day of Solidarity to Support Healthcare for Heroes
The Propel Center, the global HBCU innovation and learning hub intended to level the playing field and open greater doors of opportunity for their students, announced the creation and launch of its Propel-BDHEA internships, a national program focused on select HBCU and other African American students interested in pursuing medical and related healthcare careers. The […]
Special Olympics New York and Advance Care Alliance of New York (ACA/NY) come together to guarantee proper retrieval of healthcare services for those with intellectual and developmental disabilities. The groups come together to declare their objective of diminishing health inequalities for these groups of people by generating new opportunities. Stacey Hengsterman, President and CEO of […]

In accordance with International Living’s 31st Annual Global Retirement Index, Panama has been named the world’s #1 destination for 2022. This Index, produced in accordance with numerous statistics and on-the-ground input from in-country correspondents, ranks and rates the world’s leading retirement locations. The index surveys 10 major categories that include cost of living, retiree benefits, […]

Amidst the perseverance of the COVID-19 pandemic, the healthcare industry has taken a massive blow. There are intense staffing shortages in the field, and the public is suffering from these scarcities. The Washington Post gave a detailed report on these worsening staff deficiencies, more specifically in long term care facilities. Nursing homes tend to lessen […]
Dr. Jerome Adams, former Indiana state health commissioner and the 20th U.S. surgeon general, will join Purdue University on Friday (Oct. 1) as a Presidential Fellow and the university’s first executive director of health equity initiatives, professor of practice in the departments of Pharmacy Practice and Public Health and a faculty member of the Regenstrief […]