There is no excerpt because this is a protected post.
Posts tagged with "physicians"
The Importance of Education for Advancing Healthcare Equity
By: Maria Hernandez, Ph.D. If you’ve been tracking the nation’s progress in the fight against Covid-19, physicians and public health officials of color have been highlighting the need for health equity in the national dialogue. As the data on mortality rates becomes clearer, there is no mistake that the pandemic is impacting African American and […]
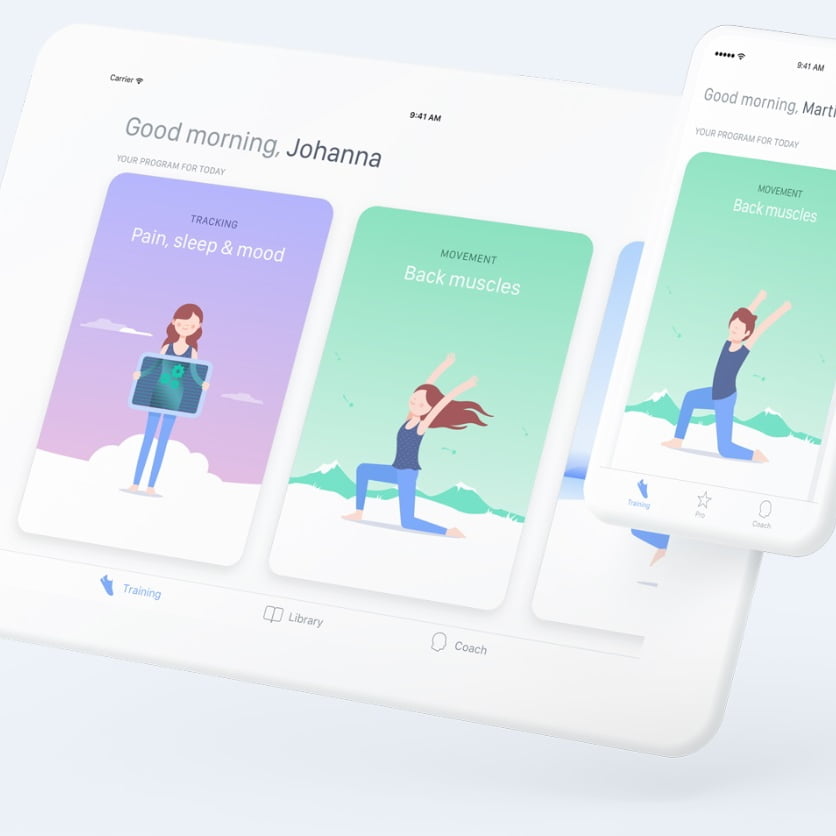
New AI app reduces back pain by 40%
Boston based digital therapy startup Kaia Health launches a new app that uses AI and patent pending motion tracking technologyto personalize treatment programs tomanage and treat chronic low back pain(LBP) which has been shown in clinical studies to reduce chronic back pain by 40% –and could save the US economy billions each year. Created by […]





